Veronika Ivanova
Bulgaria Academy of Sciences, Institute of Robotics, Bulgaria
Ani Boneva
Bulgarian Academy of Sciences, Institute of Information and Communication Technologies, Bulgaria
Vasil Metodiev
University of Chemical Technology and Metallurgy Sofia, Bulgaria
https://doi.org/10.53656/adpe-2025.11
Pages 123-137
Abstract. In recent decades, laparoscopic surgery has emerged as a standard medical procedure worldwide, gradually replacing conventional open surgery due to its numerous advantages, including reduced recovery time, lower risk of complications, and improved patient outcomes. However, in several countries, the adoption of laparoscopic techniques remains limited, primarily due to the high costs associated with advanced surgical technologies and the need for specialized training programs. There is a pressing demand for cost-effective and accessible training methodologies to equip surgeons with the necessary skills. The STEMM environment provides a valuable opportunity for training outside the operating room in a safe environment under experienced guidance without risk to patients.
The integration of STEMM principles in laparoscopic surgery has its strength in subject integration, learning in context and teaching-research activity, emphasizing the connection of learning knowledge with realities, interactivity, combining learning with game elements, reflexivity, working in a modern technological environment, and the unity of knowledge-skills-assessment. The implementation of new technologies, such as various forms of surgical simulations, in surgical training, aims to improve the learning experience, learning outcomes, patient safety, and the quality of healthcare. Here, modern surgical training methods such as simulation, VR and AR technologies robotic-assisted surgery, and haptics interface are presented, as well as their importance for acquiring good surgical skills.
This study aims to address this gap by proposing an innovative approach to laparoscopic training, integrating the principles of Science, Technology, Engineering, Mathematics, and Medicine (STEMM). By incorporating modern technologies into surgical education in an accessible and structured manner, this approach seeks to enhance the training of medical students and early-career surgeons.
Keywords: STEMM education; training, robotics, mechatronics, surgical skills
- Introduction
STEMM education represents an integrative pedagogical framework aimed at developing competencies in science, technology, engineering, mathematics, and medicine.
The field of science encompasses systematic observation, comparative analysis, experimental investigations, hypothesis formulation, causal reasoning, and the interpretation and presentation of empirical results. Technology, as a component of STEMM, focuses on problem identification, exploration of potential solutions, and the application of various tools, including both software-based and engineering solutions, to facilitate innovation and the development of utility models.
Engineering is centered on problem-solving methodologies through the selection and utilization of appropriate materials, enabling the design, planning, and construction of functional models and devices.
Mathematics plays a fundamental role in STEMM by fostering skills in measurement, pattern recognition, quantitative analysis, and geometric exploration, all of which are essential for scientific and engineering applications (Azizyan, 2025).
One of the advantages of STEMM training is the opportunity to learn outside the operating room in a controlled, risk-free environment under expert supervision. This is particularly important in medical education, where the adoption of innovative technologies improves patient safety and the quality of healthcare. The integration of simulation-based training methods is now considered a core component of modern surgical training, offering trainees the opportunity to develop procedural skills. Numerous criteria and methodologies have been proposed to improve innovative educational approaches in STEM (Trichkova-Kashamova et al., 2024), many of which are equally applicable to STEMM disciplines. In this context, emerging frameworks for integrated intelligent educational environments provide valuable opportunities for advancing STEMM education (Terzieva et al., 2024).
Technology is increasingly pervasive in all aspects of education and professional training. Digital innovations facilitate the modeling of new learning approaches and encourage dynamic interactions between learners, educators, and industry professionals. The diverse range of technological applications in STEMM education includes online interactive learning platforms, simulation-based learning, augmented and virtual reality (AR/VR), training, and more. These improvements contribute to the effective preparation of future specialists and doctors
Robotics, Mechatronics, artificial intelligence, and virtual and Additional intelligence are all STEAM-based opportunities.
This section aims to explore the application of advanced technologies such as augmented reality (AR), virtual reality (VR), haptic interfaces, robotics, mechatronics, and contemporary healthcare innovations as effective tools for education and professional skill development.
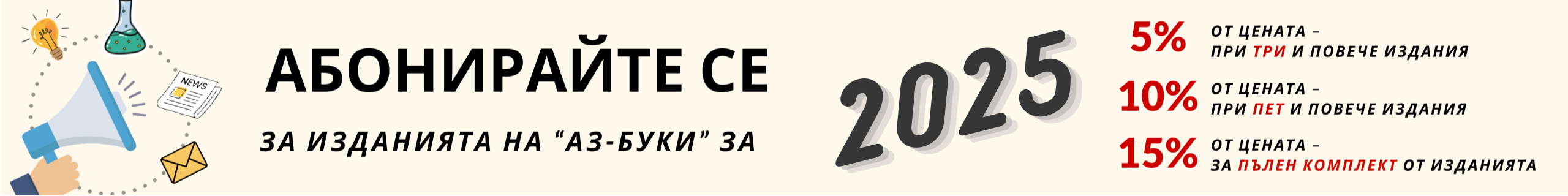
The systematically classified fundamental approaches to laparoscopic skills training are preseted, providing a structured framework for the development of proficiency in minimally invasive surgical techniques. These foundational methods serve as the basis for structured training programs, to which additional essential techniques and innovative methodologies can be integrated (Fig. 1).
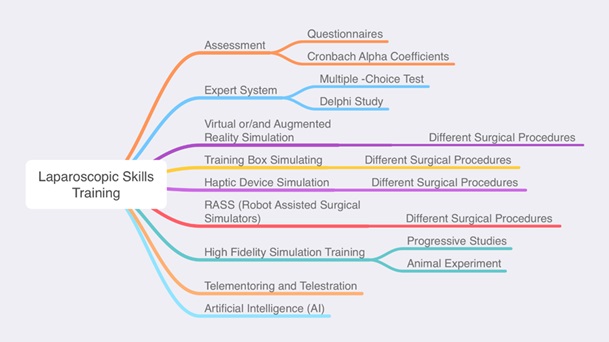
Figure 1. Laparoscopic Skills Training
1.1. The STEMM principles
STEMM education is fundamentally grounded in research, discovery, and experiential learning. The emphasis is on practical engagement, ensuring that acquired knowledge and skills can be directly applied to real-world scenarios. This hands-on approach facilitates a more intuitive, accelerated, and effective learning process, often incorporating game-based learning and experimental activities that stimulate curiosity and problem-solving abilities.
From a disciplinary perspective, STEMM encompasses a diverse range of scientific and technological fields, each contributing to the study of natural phenomena and the development of innovative solutions to real-world challenges. This multidisciplinary integration fosters the accumulation of competencies that enable learners to apply their theoretical understanding to practical problem-solving. The pedagogical framework of STEMM education follows a „learning-by-doing“ methodology, where instruction is structured to move from practice to theory, reinforcing applied learning.
The integration of STEMM principles into education is facilitated through a variety of interactive and engaging formats, including educational projects, hands-on experiments, specialized training programs, and more.
For example, training sessions emphasize hands-on practice, offering a wide range of topics and diverse implementation strategies tailored to real-world applications. Meanwhile, lectures within STEMM education retain elements of traditional teaching methods but are structured to be interactive and participatory. This blended approach combines theoretical and practical components, requiring active engagement of learners. Through such dynamic learning models, students are given opportunities to explore new knowledge, hone technical skills, and develop competencies that are essential for solving contemporary scientific and technological challenges. The workshop is a place where hands-on work, modeling and construction are done. STEMM – the lesson is a form of learning, but in a specific and characteristic way for STEMM, respecting the requirement for integration of the four sciences: technology, science, engineering, mathematics and medicine,
Another STEMM form is the center – which unites different premises according to the learning modes, and here the emphasis is on the arrangement of the environment, which was discussed earlier in this article.
Specialists in the center apply teaching methods that encourage creative and critical thinking in students. Activities related to visiting and touching real professionals from different fields and contact with their workplaces, tools and accessories, the buildings in which they work for the benefit of society – doctor, dentist, etc., would create a desire for career guidance (Borisova, 2023).
The integration of science, technology, engineering, mathematics and medicine (STEMM) principles for the development of good Laparoscopic skills training is a key element. The main goal of the work is to apply a modern approach through STEMM education integrating modern technologies in a convenient way for students and young doctors, which will ensure the preparation of a new generation of surgeons and stimulate progress in medicine for better care of people. Here we will try to present the application of AR, VR, haptic interface, robotics, mechatronics, and current health technologies, as a convenient means for this training. For this reason, the following is done: STEMM Education in Laparoscopy is presented. In Methods and tools for training, the possibilities of modern training tools are considered. Then Challenges and possibilities, trends and future directions of STEMM education in Laparoscopy are presented.
- Enhancing Laparoscopic Training Through STEMM Integration
The learning curve in laparoscopy is step-like, as several stages of training are overcome, such as the transition from two-dimensional to three-dimensional observation of the working space, etc. This includes lecture courses and laboratory exercises with the use of computerized simulators, tissues with properties close to human ones, which ensures good efficiency for training skills. The use of simulators, as well as training in virtual and augmented reality, are important for the adequate acquisition of these skills. The FLS (Fundamental of Laparoscopic Surgery) program is a validated educational tool that includes web-based materials and physical simulators for teaching and assessing basic laparoscopic skills. This program ensures that trainees meet high educational standards through rigorous validation processes (Vassiliou et al., 2010; Fried, 2008). The goal is to provide practicing physicians an opportunity to learn the fundamentals of laparoscopic surgery in a consistent, scientifically accepted format; and to test cognitive, surgical decision-making, and technical skills, all with the goal of improving the quality of patient care (American Board of Obstetrics & Gynecology, 2025).
Developing a structured laparoscopic training program is essential for ensuring systematic skill acquisition and competency development in minimally invasive surgery (MIS). A well-designed curriculum must define clear learning objectives, progressive milestones, and assessment criteria to evaluate proficiency at different stages of training. The following framework provides a structured approach to laparoscopic education, ensuring that trainees master foundational skills before advancing to more complex surgical procedures.
Participants in the training are assessed on basic laparoscopic tasks using a global rating scale and a checklist for specific tasks. The assessment can be in the form of Questionnaires, Cronbach Alpha Coefficients, etc. Participants are then trained under the supervision of an instructor and then assessed using the same global rating scale and checklist for specific tasks. Participants perform a basic procedure on a live animal (pig) on the second day of training and are assessed again (Sihombing et al., 2017). The application of Expert systems in diagnosis and assessment – Multiple-Choice system, Delphi Study etc.
Knowledge acquisition is important in building knowledge-based systems. It is necessary to extract and integrate knowledge from multiple experts to build an effective expert system. Multiple expert systems may have different expertise and knowledge in the same application domain. The expert systems can be effective in dealing with medical diagnostic problems. The Delphi-based approach plays an important role in extracting knowledge from multiple experts. An application for the diagnosis of severe acute respiratory syndrome illustrates the superiority of this approach (Chu & Hwang, 2008). The Delphi Study has been successfully applied to assess surgical skills in suturing, reflecting expert-level performance (Mathis et al., 2020). Multiple-Choice system is a form of an objective assessment in which respondents are asked to select only the correct answer from the choices offered as a list. The multiple-choice format is most frequently used in educational testing (Park, 2010; Tan & Mcaleer, 2008).
Ethical and Practical Considerations
As laparoscopic training methods are refined, ethical and practical considerations must be taken into account. Ensuring equitable access to high-quality training resources and simulators across institutions is vital. Furthermore, the costs associated with advanced simulation technology pose a significant challenge, especially in resource-limited settings.
- Training Methods and Tools
Simulation has emerged as a major tool for laparoscopic training. High-fidelity simulators provide a risk-free environment in which surgical skills are practiced and honed. To reduce training time, a wide variety of simulators are used, from basic simulators that reproduce the laparoscopic environment to advanced virtual reality (VR) simulators. Fig. 2 shows a schematic diagram of the main classification of surgical simulators (Häberle et al., 2023).
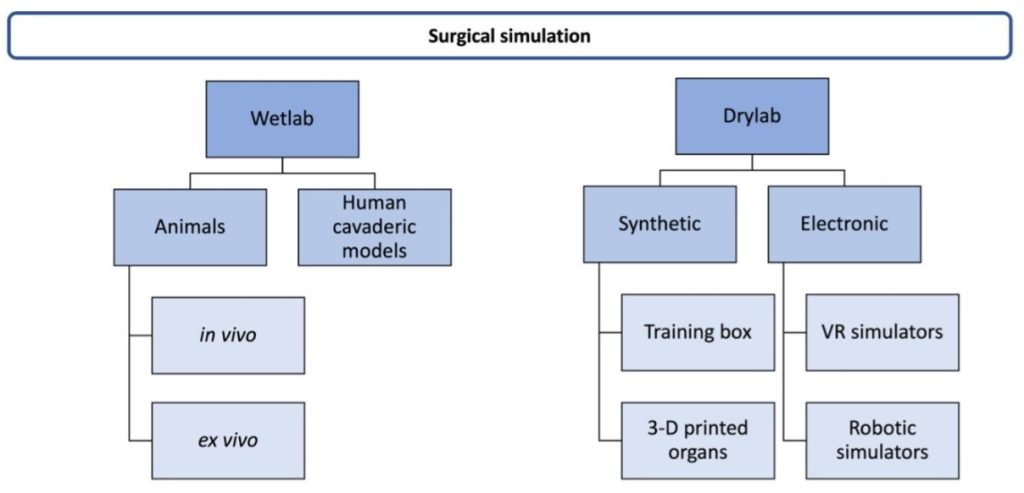
Figure 2. Classification of surgical simulators (Häberle et al., 2023)
The latter have proven to be an advanced and effective training method that significantly improves the surgeon’s skills in the operating room. The use of VR in training not only helps in the acquisition of skills, but also in the objective assessment of the competence of the trainees. Simulators allow for the achievement of the maximum level of realism and emulation of complex procedures.
Also, simulation is a suitable method for training surgeons in the acquisition of complex movements and operations, as it reduces the duration of training. With the help of simulation, the force of interaction between the instrument and the tissue is optimized.
Both computerized simulators and tissue and cadaver simulators are used for the effective acquisition of surgical skills. This is a preferred approach for training surgeons and in recent years there has been pressure to include it as a mandatory subject in surgical training programs.
3.1. Training boxes
They are a fairly common surgical training simulator. Their advantage is the reduction of training time. This is a preferred training method in countries with low budgets and less than ideal training conditions. Before training with training boxes, lectures are given consisting of basic instruments and techniques. Then, a demonstration is made by the instructor for tasks. This is followed by an exercise in which participants perform several tasks. This is followed by a demonstration of skills on a pig.
Many users cannot effectively use training boxes due to the requirement for an additional monitor, connecting cable and power source. These disadvantages are overcome with a new generation of training boxes, where visualization is performed directly via a personal smartphone/tablet (Uruç et al., 2018).
Incorporating 3D visualization into 2D laparoscopic training in training boxes can accelerate skill acquisition, reducing training time.
3.2. Advanced methods-VR and AR technologies, robotic-assisted surgery, Haptic interface
VR simulators are being applied in medical practice with increasing positive results. Some have already proven the benefits of using VR simulators in laparoscopic surgery (Queirós et al., 2012; Larsen et al., 2009; Gurusamy et al., 2009), contributing to the improvement of surgical skills. So far, some simulators such as Lap Mentor, ProMIS, LapSim, SimSurgery, LAGB or LTS3e. provide VR, allow training of skills, knowledge and judgment for laparoscopic surgery (Ayodeji et al., 2007; Buzink et al., 2010). They are a powerful tool in the training and assessment of promising- Virtual reality training is more successful with individual training and a developed schedule for mastering certain skills. The limitations of loss of tactility when working with tools and the fulcrum effect impose the requirement for an opposing motion.
Virtual reality-based simulators can use an application that allows for interactive exploration of 3D anatomical models and animations. Virtual reality is applicable through developed mobile applications to explore various surgical approaches using a smartphone or tablet. Each virtual study uses 3D anatomical models and animations. A training system aimed at mastering the method of positioning the patient according to a specific anatomy and a specific goal is interesting. The study of each approach in 3D mode can also be divided into phases. VR simulators allow trainees to practice individual movements or entire procedures in a near-real environment. Modern VR simulators can reproduce complex minimally invasive surgery by measuring various parameters of the procedure, including movement efficiency and node reliability, time to perform the operation, even remote assessment of effectiveness.
The cost of the simulators is quite high and they do not have tactile feedback and lack realism. Some authors show a virtual simulator for suturing pre-wound soft tissues without showing the knotting, which is a key point in suturing (Lian & Chen, 2006).
3.3. Augmented Reality
Advanced medical technology is related to obtaining real-time information and data and their visualization, as their use makes diagnosis and treatment faster and more reliable, and training more effective. Augmented reality surgical systems and devices allow doctors to visualize data from diagnostic and surgical procedures and improve work efficiency. The basic principle of augmented reality is the superimposition of computer-generated (CG) images on real images captured by a camera and then displayed on a computer, tablet or video projector.
Model libraries can serve different platforms and allow high-resolution, high-resolution 3D visualizations, which in turn allows the implementation of augmented reality applications, including for training. The main advantage is that the surgeon is not limited to looking away from the surgical site, unlike conventional imaging techniques. The Augmented Reality technique allows visualization of blood vessels, nerves and vital tissues. It is also possible to control the opacity of the images being viewed. Surgical simulation, combined with virtual, mixed and augmented reality, has become increasingly popular. AR is a technology in which digital information does not interact with the real environment, but is superimposed on the user’s view of the external environment as graphics, audio or video information.
The communication task of transmitting the video signal from the operating field to one or more participants in the training, as well as the control signals to the actuators of robotic laparoscopic components, can be solved by many of the currently available wireless communication standards and their technological implementations – Wi-Fi 6 and 6E (IEEE Standard For Information Technology, 2021; IEEE Standard For Information Technology, 2022), Wi-Fi 7 (IEEE Standard For Information Technology, 2024). Table 1. presents some of the possible scenarios for the application of these technologies in the training processes for laparoscopic surgery.
Table 1. Possible Scenarios of Technologies in the Training for Laparoscopic Surgery
| Communication bandwidth requirements, Mbps per user | Network end to end latency, ms | Network jitter, ms | Packet delivery reliability, % | |
| Recorded operation simulation | 20 | < 50ms | < 5 ms | 99.99% |
| VR 360 live broadcasting | ||||
| AR visualization | ||||
| Interactive operation simulation | 100 | < 15 ms | < 5 ms | 99.99% |
| Panoramic live broadcast | ||||
| Cloud-assisted 4K+ simulation | 400 | < 10 ms | < 5ms | 99.99% |
| VR remote motion control for surgery | ||||
| AI-assisted smart helmet/glasses | 30 | < 20 ms | < 1 ms | 99.999% |
| Real-time command for remote surgery |
Table 2. presents a comparative analysis of the applicability of current Wi-Fi 6, Wi-Fi 6E and Wi-Fi 7 wireless technologies in the context of applicability in laparoscopic surgery, with an emphasis on remote AR/VR assisted observation of processes by many participants and remote control of manipulators by an instructor.
Table 2. Comparative Analysis OF THE Applicability of WI-FI 6, WI-FI 6E and WI-FI 7
| Criteria | Wi-Fi 6 | Wi-Fi 6E | Wi-Fi 7 |
| (IEEE 802.11ax) | (IEEE 802.11ax + 6GHz ISM band) | (IEEE 802.11be) | |
| Price | Low | Moderate | High |
| Bandwidth per user | ~ 1-2 Gbps (theoretical 9.6 Gbps aggregate) | ~ 2-4 Gbps (additional 6GHz spectrum reduces congestion) | ~ 5-10 Gbps (320 MHz channels, Multi-Link Operation) |
| End-to-End Latency | 10-20 ms | 10-20 ms | < 5ms |
| (MLO, lower PHY latency) | |||
| Jitter | Moderate | Low | Very Low |
| (high in crowded 2.4/5GHz bands) | (clean 6GHz spectrum) | (MLO minimizes variability) | |
| Reliability | Moderate (prone to interference) | High (dedicated 6GHz channels) | Very High (MLO, preamble puncturing, 4096-QAM) |
Table 3. presents the summarized capabilities of the three wireless standards for application in AR/VR technologies for laparoscopic surgery and training.
Table 3. Summary Capabilities of WI-FI 6, WI-FI 6E and WI-FI 7
| Role | Wi-Fi 6 | Wi-Fi 6E | Wi-Fi 7 |
| Remote Viewing | Risk of congestion in dense 5 GHz environments; suitable only for smaller teams or lower-resolution streams. | Best balance for high-resolution streaming (6 GHz reduces congestion, ensuring stable bandwidth for multiple users). | Ideal for ultra-high-definition feeds (e.g., 8K/360° video) with its massive bandwidth and MLO redundancy. |
| (Multiple Participants) | |||
| Remote Robotic Control | Not recommended due to higher latency/jitter in crowded networks (risk of delayed robotic response). | Viable alternative with dedicated 6 GHz channels but lacks MLO’s redundancy. | Critical for sub-5 ms latency and ultra-reliable connections (MLO ensures failover if one band drops). |
| (Single teacher) | |||
| Applicability and recommendations | Legacy Systems: Wi-Fi 6 can suffice for non-critical remote viewing if network load is managed tightly. | Budget-Conscious: Use Wi-Fi 6E for its 6 GHz spectrum (avoids 5 GHz congestion) at a moderate cost. | High-Risk Robotic Control: Invest in Wi-Fi 7 for mission-critical reliability and latency. |
The high accuracy of the simulator allows visualization of various tissues, tumors, arteries, and veins A designed model with set parameters characterized is shown in Fig 3.
Figure 3. A designed models with set parameters characterized by the physical properties of actual organs and various tissues, tumors, arteries, and veins
The skin, blood vessels, organs and ribs are rendered to enhance realism and can be set to be transparent or hidden. The virtual organs in the thoracic and abdominal cavities are simulated and are presented in accordance with the patient’s CT scan data. Surgical trainees can zoom in and observe the simulated patient’s organs from different angles in this way. One of the biggest difficulties in laparoscopic surgery is the lack of sensitivity. When performing surgery, the observation is performed on a flat 2D screen, it is difficult to judge the depth of penetration, etc.
Therefore, we use a specially developed laparoscopic tool for a robot for this training module, which can be applied to train depth perception and a method with macro and micro segmentation (Ivanova et al., 2020) to obtain the range of the force.
3.4. Telestration and Augmented Reality
Creating augmented reality (AR) telestration models to support intraoperative expert guidance and training in MIS is one of the latest trends in the field of surgical education. AR telestration models have shown positive results in acquiring basic laparoscopic skills. In addition, AR telestration models can provide effective MIS training and real-time intraoperative guidance during MIS procedures also remotely.
3.5. Robotic-Assisted Surgery (RAS)
Robotic-Assisted Surgery has some advantages over laparoscopic surgery, as it restores some of the visualization through 3D stereoscopic observation, facilitates instrument manipulation, and provides a stable platform and advantages for precise dissection, accurate trajectory tracking, and manipulation. Some RAS systems have eye tracking and tremor filtering features, which allow the surgeon to be more precise. RAS includes a surgical digitization platform, allowing for the extraction of surgical data as well as the input of various types of information to support the surgical performance. RAS potentially reduces the workload and shortens the surgical learning curve compared to conventional laparoscopy. RAS is currently widely used in various surgical disciplines, such as urology, gynecology, general and cardiothoracic surgery. Most RAS training focuses on developing the technical and cognitive skills required to operate the surgical console, and some also provide full procedural simulations. Some of the most widely used RASS simulators are SEP-Robot, RoSS, RobotiX Mentor dV-Trainer and da Vinci Skills Simulator.
VR simulators integrated with haptic interfaces incorporating tactile and force feedback to simulate surgical scenarios have shown good results in training (Panait et al., 2009). As a disadvantage, such interfaces are expensive, making them unsuitable for small and medium-sized hospitals or private use.
3.6. Haptic interface
In recent decades, computer-aided technologies with integrated haptic devices have been used to train surgeons. The application of simulators incorporating force feedback in a simulated surgical environment would allow for superior performance of the trainee compared to repeating the same basic skill tasks in a non-haptic environment. For difficult tasks, training with laparoscopic simulators equipped with haptics allows for superior precision, leading to faster task completion and a tendency towards fewer technical errors.
The potential benefits of virtual surgery are extensive: cost reduction, objective assessment of surgical skills, reduced risk to patients as the surgeon progresses.
Simulators should provide features that truly train and improve surgeon skills, such as physician assessment and surgeon skill improvement assessment.
It is worth considering the evaluation of the system for effectiveness, accuracy, or robustness, as well as the evaluation methodologies. Important in this type of training are the basic functions of a laparoscopic surgery simulation system, including organ modeling, visual imaging, and haptic imaging in a multifaceted application. Several specific task-procedures, such as deep learning and cutting, are designed to train physician skills and are also of interest in this training.
Telementoring and telestration. Telementoring, facilitated by advances in telecommunications, allows experienced surgeons to guide trainees remotely during laparoscopic procedures. Telestration, which involves the superimposition of digital markers on the video stream, enhances this interactive learning experience.
This method not only expands access to expert guidance, but also facilitates a collaborative learning environment.
3.7. Integration of Artificial Intelligence
Artificial intelligence (AI) in laparoscopic training is a relatively new and modern trend. AI algorithms can analyze surgical videos, providing feedback on technique, efficiency, and error rates. This technology promises personalized training modules and predictive analytics to identify areas for improvement, tailoring training to individual needs (World Laparoscopy Hospital, 2023).
- Challenges and Possibilities, Trends and Future Directions of STEMM Education in Laparoscopy
Limited observation in certain regions of the surgical field is hampered by factors such as lack of training, expert trainers, and equipment, highlighting the challenges in implementing laparoscopic training programs in certain settings (Sánchez-Margallo et al., 2014).
A study in surgical departments in Switzerland shows that the existing curriculum does not meet the requirements of a modern curriculum, which in turn necessitates the creation of an improved, adequate curriculum for training a new generation of surgeons (Klempous et al., 2015). Simulator-based training in laparoscopy involves transferring acquired knowledge and skills from the training room to the operating room, aiming to extract the best, to prepare structured target training courses and to reach a predetermined level of competence.
As a future direction, the development and implementation of pan-European standards for training in laparoscopic surgery can be considered, as a result of which the quality of the offered clinical services and education will be increased
Introduction of a method for measuring competence with laparoscopic techniques, which indicates a shift towards more standardized training and assessment in laparoscopy.
The future of training in laparoscopic surgery should be guided by continuous innovation. Augmented Reality (AR), providing real-time overlays of anatomical structures and critical information during surgery. Integration of haptic feedback in simulators offering tactile sensations ensures a good training experience. Furthermore, the introduction of joint international training programs through virtual platforms can further develop the possibilities of surgical education.
- Conclusions
This article presents a comprehensive vision for enhancing laparoscopic surgery training by incorporating modern training methodologies and STEMM (Science, Technology, Engineering, Mathematics, and Medicine) principles into laparoscopic skill acquisition. The integration of simulation-based learning, structured curricula, tele-tutoring, and advanced technologies such as Artificial Intelligence (AI) and Augmented Reality (AR) represents a transformative approach to surgical education.
As surgical techniques and technologies continue to evolve, it is imperative that surgical training methodologies undergo concurrent advancements to uphold the highest standards of patient care and surgical proficiency.
By leveraging interdisciplinary STEMM-driven approaches, laparoscopic education can be optimized to provide surgeons with enhanced technical skills, improved decision-making abilities, and real-time adaptive learning experiences.
American Board of Obstetrics & Gynecology. (2025). Fundamentals of Laparoscopic Surgery (FLS). https://www.abog.org/specialty-certification/surgical-skills-program-standard/fundamentals-of-laparoscopic-surgery-fls.
Ayodeji, I., Schijven, M., Jakimowicz, J., Greve, J. (2007). Face validation of the Simbionix LAP Mentor virtual reality training module and its applicability in the surgical curriculum, Surgical Endoscopy, 21(9), 1641 – 1649. https://doi.org/10.1007/s00464-007-9219-7.
Azizyan, K. (2025). STEM – everything we need to know about it. Prepodavame.bg. https://prepodavame.bg/stem-kakvo-tryabva-da-znaem-za-nego/. [in Bulgarian]
Borisova, P. (2023). STEM forms-a way to integrate the interdisciplinary approach into the Bulgarian education system. Е-Journal Pedagogical Forum, 1, 176 – 181. [in Bulgarian].
Buzink, S. N., Goossens, R. H. M., Ridder, H. D., Jakimowicz, J. J. (2010). Training of basic laparoscopy skills on SimSurgery SEP. Minimally Invasive Therapy & Allied Technologies, 19(1), 35 – 41. https://doi.org/10.3109/13645700903384468.
Chu, H-C., Hwang, G-J. (2008). A Delphi-based approach to developing expert systems with the cooperation of multiple experts. Expert Systems with Applications, 34(4), 2826 – 2840. https://doi.org/10.1016/j.eswa.2007.05.034.
Fried, G. M. (2008). FLS Assessment of Competency Using Simulated Laparoscopic Tasks. Journal of Gastrointestinal Surgery, 12(2), 210 – 212. https://doi.org/10.1007/s11605-007-0355-0.
Gurusamy, K. S., Aggarwal, R., Palanivelu, L., Davidson, B. R. (2009). Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Systematic Reviews, 21(1). https://doi.org/10.1002/14651858.cd006575.pub2.
Häberle, F., Cizmic, A., Cizmic, A. (2023, 28 Mart). Modern Digital Technologies in Surgical Training. Swiss College of Surgeons. https://www.swiss-knife.org/pdf/download/934
IEEE Standard for Information Technology. (2021). Telecommunications and Information Exchange between Systems – Local and Metropolitan Area Networks—Specific Requirements. Part 11: Wireless LAN Medium Access Control (MAC) and Physical Layer (PHY) Specifications – Amendment 1: Enhancements for High Efficiency WLAN (IEEE 802.11ax-2021). https://standards.ieee.org/ieee/802.11ax/.
IEEE Standard for Information Technology. (2022). Telecommunications and Information Exchange between Systems – Local and Metropolitan Area Networks – Specific Requirements. Part 11: Wireless LAN Medium Access Control (MAC) and Physical Layer (PHY) Specifications – Amendment 2: Enhanced Operation in the 6 GHz Band (IEEE 802.11ax-2021/Amd 2-2022). https://standards.ieee.org/ieee/802.11ax/.
IEEE Standard for Information Technology. (2024). Telecommunications and Information Exchange between Systems – Local and Metropolitan Area Networks – Specific Requirements. Part 11: Wireless LAN Medium Access Control (MAC) and Physical Layer (PHY) Specifications – Amendment 8: Enhancements for Extremely High Throughput (EHT) (IEEE 802.11be-2024). https://standards.ieee.org/ieee/802.11be/.
Ivanova, V., Bachvarov, D., Boneva, A. (2020). A Smart Laparoscopic Instrument with Different Applications. International Journal of Bioautomation, 24(4), 403 – 417. https://doi.org/10.7546/ijba.2020.24.4.000723.
Klempous, R., Nikodem, J., Wytyczak-Partyka, A. (2015). Computer-assisted surgical trainer for minimally invasive surgery”. IEEE 10th Jubilee International Symposium on Applied Computational Intelligence and Informatics, 541 – 545. https://doi.org/10.1109/SACI.2015.7208263.
Larsen, C. H., Soerensen, J. L., Grantcharov, T. P., Dalsgaard, T., Schouenborg, L., Ottosen, C., Schroeder, T. V., Ottesen, B. S. (2009). Effect of virtual reality training on laparoscopic surgery: randomised controlled trial. British Medical Journal (BMJ), 338, 1 – 6. DOI: https://doi.org/10.1136/bmj.b1802.
Lian, L., Chen, Y. H. (2006). Haptic surgical simulation: An application to virtual suture. Computer-Aided Design & Applications, 3(1 – 4), 203 – 210. https://doi.org/10.1080/16864360.2006.10738457.
Mathis, R., Watanabe, Y., Ghaderi, I., Nepomnayshy, D. (2020). What are the skills that represented expert-level laparoscopic suturing? A Delphi Study. Journal Surgical Endoscopy, 34(3), 1318 – 1323. https://doi.org/10.1007/s00464-019-06904-w.
Panait, L., Akkary, E., Bell, R. L., Roberts, K. E., Dudrick, S. J., Duffy, A. J. (2009). The role of haptic feedback in laparoscopic simulation training. Journal of Surgical Research, 156, 312 – 316. https://doi.org/10.1016/j.jss.2009.04.018.
Park, J. (2010). Constructive multiple-choice testing system. British Journal of Educational Technology, 41(6), 1054 – 1064. https://doi.org/10.1111/j.1467-8535.2010.01058.x.
Queirós, S. F., Vilaça, J. L., Rodrigues, N. F., Neves, S. C., Teixeira, P. M., Correia-Pinto, J. (2012). A laparoscopic surgery training interface. IEEE 1st International Conference on Serious Games and Applications for Health (SeGAH). https://doi.org/10.1109/SeGAH.2011.6165446.
Sánchez-Margallo, J. A., Sánchez-Margallo, F. M., Oropesa, I., Aguilera, E. J. G. (2014). Systems and technologies for objective evaluation of technical skills in laparoscopic surgery. Minimally Invasive Therapy & Allied Technologies, 23(1), 40 – 51. https://doi.org/10.3109/13645706.2013.827122.
Sihombing, A. T., Sibarani, J., Adi, S. (2017). Effectiveness of Low Cost Laparoscopic Training Box to Increase Laparoscopic Skills in Urology Training Center Universitas Padjadjaran/Hasan Sadikin General Hospital. Open Access Library Journal, 4(3), 1 – 10. https://doi.org/10.4236/oalib.1103412.
Tan, L.T., Mcaleer, J. J. A. (2008). The introduction of single best answer questions as a test of knowledge in the final examination for the fellowship of the Royal College of Radiologists in Clinical Oncology. Clinical Oncology, 20(8), 571 – 576. https://doi.org/10.1016/j.clon.2008.05.010.
Terzieva, V., Ilchev, S., Djambazova, E. (2024). Integrated Intelligent Educational Environment – Opportunities for STEM Education. IFAC-Papers OnLine, 58(3), 94 – 99. https://doi.org/10.1016/j.ifacol.2024.07.132.
Trichkova-Kashamova, E., Paunova-Hubenova, E., Boneva, Y., Dimitrov, S. (2024). Criteria and Approaches for Optimization of Innovative Methods for STEM Education. IFAC-PapersOnLine, 58(3), 123 – 128. https://doi.org/10.1016/j.ifacol.2024.07.137.
Uruç, F., Akan, S., Aras, B., Uruç, E., Verit, A. (2018). No-cable and smartphone/tablet: A functional laparoscopic training box “Fu-Lap T-Box”. Turkish Journal of Urology, 44(5), 428 – 431. https://doi.org/10.5152/tud.2018.56313.
Vassiliou, M. C., Dunkin, B. J., Marks, J. M., Fried, G. M. (2010). FLS and FES: Comprehensive Models of Training and Assessment. Surgical Clinics of North America, 90(3), 535 – 558. https://doi.org/10.1016/j.suc.2010.02.012.
World Laparoscopy Hospital. (2023, 26 December). Enhancing Surgical Education: Laparoscopic Training Methods. https://www.laparoscopyhospital.com/worldlaparoscopyhospital/index.php?pid=429?p%3D5.
Assist. Prof. Veronika Ivanova, PhD
ORCID iD: 0000-0002-6033-3988
Web of Science Researcher ID: JEP-2931-2023
Bulgaria Academy of Sciences Institute of Robotics,
Sofia, Bulgaria
E-mail: iwanowa.w@abv.bg
MSc. Eng. Ani Boneva
ORCID iD: 0000-0002-1743-1638
Web of Science Researcher ID: X-1955-2018
Bulgarian Academy of Sciences Sofia, Institute of Information and Communication Technologies
Sofia, Bulgaria
E-mail: ani.boneva@iict.bas.bg
Assist. Prof. Vasil Metodiev, PhD
ORCID iD: 0000-0002-5773-0894
Web of Science Researcher ID: ABM-5550-2022
University of Chemical Technology and Metallurgy
Sofia, Bulgaria
E-mail: metodiev@uctm.edu